Opportunistic Infections and Factors Influencing Immune Vulnerability
Opportunistic infections refer to infections caused by microorganisms that, in healthy individuals, are either part of the normal flora or do not pose a threat to cause diseases. However, they seize the opportunity to induce infections when an individual’s immune system is compromised. These microorganisms, also known as opportunistic organisms or opportunistic pathogens, become infectious when the individual’s immunity weakens.
Immune compromise occurs when various factors impact the integrity and functionality of the immune system, rendering the individual susceptible to infections. These influencing factors are diverse and can include the impairment of skin and mucosal integrity, neutropenia, diabetes, AIDS, chemotherapy, lymphopenia, deficiencies in immunoglobulins and complement, as well as the negative progression of one or more biological, sociocultural, and environmental factors. Opportunistic pathogens take advantage of such situations, causing various diseases in individuals.
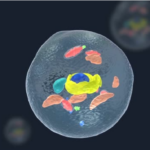
These pathogens fall into four main categories: bacteria, viruses, parasites, and fungi. They act opportunistically, capitalizing on the weakened defense mechanisms brought about by compromised immunity. Factors such as disruptions in the skin-mucosa barrier, neutropenia, diabetes, AIDS, chemotherapy, lymphopenia, immunoglobulin deficiencies, complement deficiencies, and the negative impact of sociocultural and environmental factors create an environment conducive to opportunistic infections.
Understanding opportunistic infections and the factors that contribute to immune vulnerability is crucial for effective prevention and management strategies. Comprehensive measures addressing both biological and environmental aspects are essential to minimize the risk of opportunistic infections and enhance overall health outcomes.
Opportunistic Pathogens: Bacterial Culprits and Their Impact on Immunosuppressed Individuals
Bacteria
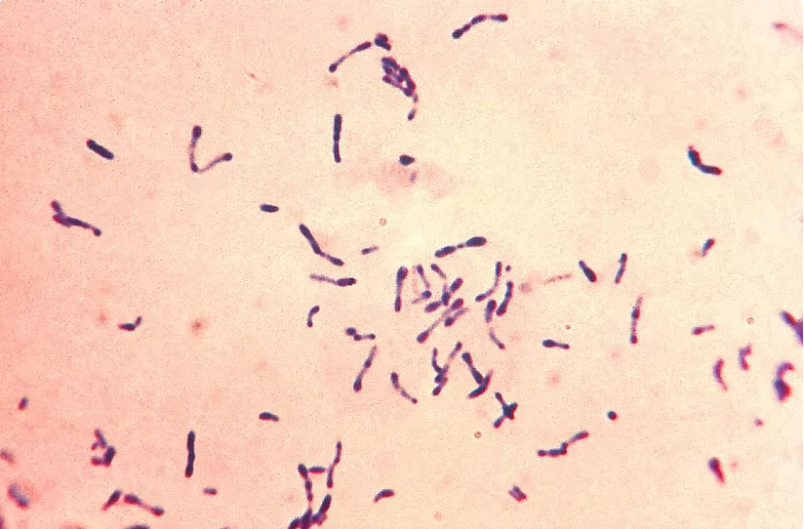
Bacteria are often the instigators of opportunistic infections in individuals with suppressed immune systems. Among these microorganisms, Pseudomonas aeruginosa, Streptococci, Nocardia spp., Staphylococcus spp, Corynebacterium spp., Salmonella spp., Bacillus spp., Legionella spp., and Listeria spp. are commonly encountered.
Pseudomonas aeruginosa and Streptococci
Pseudomonas aeruginosa is a gram-negative, non-spore-forming, encapsulated bacterium. It serves as an opportunistic pathogen in individuals with compromised immunity, affecting respiratory and urinary tracts, burns, open wounds, and can also lead to bloodstream infections. Approximately one-tenth of nosocomial (hospital-acquired) infections are attributed to P. aeruginosa. Cystic fibrosis patients are particularly susceptible to P. aeruginosa infections. In addition, exposure to conditions with low water quality, such as contaminated tubs and jacuzzis, can lead to dermatitis caused by P. aeruginosa.

Streptococci are generally Gram-positive organisms seen in chains or pairs, facultative anaerobic catalase-negative bacteria. The use of mucotoxic drugs in leukemia patients often results in mucosal damage. The compromised mucosa creates a conducive environment for the development of Streptococcal infections, particularly in conjunction with Pseudomonas aeruginosa in cases where mucosal damage occurs.
Understanding the characteristics and implications of these opportunistic bacterial pathogens is crucial for managing infections in immunocompromised individuals. Vigilant monitoring and tailored preventive measures are essential in healthcare settings to minimize the impact of these bacterial culprits on vulnerable populations.
Staphylococcus And Corynebacterium
One of the major challenges associated with immunosuppressed patients is their dependency on the bed and the presence of invasive devices, such as catheters, in their bodies. Intravenous catheters serve as entry points for bacteria like Staphylococcus spp. and Corynebacterium spp. These catheters also provide a suitable surface for microorganisms to adhere to. Remarkably, microorganisms can attach to the catheter surface within two hours of insertion. By the 18th hour, they progress to covering the entire surface, multiplying within a polymeric matrix that protects them from antimicrobial drugs and adverse environmental conditions. This complex structure is known as a biofilm, and biofilms are a critical factor negatively influencing the success of treatment. Staphylococcal bacteria and Corynebacterium spp. are among the most common bacterial species contributing to these challenges. Understanding the dynamics of these bacteria and biofilm formation is crucial for devising effective strategies to mitigate the impact on immunocompromised individuals with invasive medical devices.
A Common Opportunistic Pathogen in Cancer Patients
Listeria monocytogenes stands out as the most frequent opportunistic pathogen causing central nervous system infections in cancer patients. This disease is foodborne in nature. In a comprehensive review by Long and Koyhman (2016), who focused on post-transplantation infections, bacterial infections were identified as the most commonly encountered infections following transplantation. They specifically noted that infections following renal transplantation are the most prevalent among solid organ transplantations. Urinary system infections were highlighted as the most common type after renal transplantation, with fever being the most prominent symptom during their development.
Post-transplantation indications are categorized into three groups. In the initial post-transplantation period of 1 month, patients commonly experience pain related to the surgical site. Between 1 and 6 months, immunosuppression initiates, paving the way for opportunistic infections. Beyond the 6-month mark, these infections transition from an acute phase to a chronic phase. Although transplantation-related infections often lead to the development of bacteremia, viruses directly associated with transplantation have already secured their place in textbooks and literature.
Insights into Infections Post-Transplantation
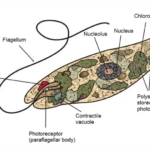
Viruses constitute another significant group of microorganisms frequently associated with opportunistic infections. Notable infectious agents in this group include Cytomegalovirus (CMV), Epstein-Barr Virus (EBV), BK Virus (BKV), Adenoviruses, and Herpes Simplex Virus (HSV).
CMV, EBV, BKV, and Adenoviruses particularly manifest and pose serious problems in patients undergoing bone marrow transplantation.
HSV, commonly known for causing cold sores, remains latent in nerve cells and tends to manifest as shingles during periods of weakened immunity, such as in times of stress or sadness. Additionally, HSV serves as a significant infectious agent in neutropenic patients as an opportunistic pathogen. Jordan et al. (2016) conducted a study investigating infections occurring after renal transplantation in pediatric patients. CMV, EBV, and BKV are infections that develop after solid organ transplantation. While there is sufficient literature for adults on this subject, information regarding pediatric patients is limited.
Therefore, Jordan and colleagues conducted a study to identify potential risk factors for the development of CMV, CMV, and BKV in pediatric patients after kidney transplantation. Age, gender, race, co-infections with seasonal pathogens, and neutropenia were identified as risk factors for post-transplantation indications. They also emphasized the need for further research on certain aspects of the topic.
Opportunistic Pathogens in Immunocompromised Individuals
Fungi such as Pneumocystis jiroveci, Aspergillus fumigatus, Aspergillus flavus, Cryptococcus neoformans, and Candida spp. are known to cause infections in individuals with weakened immune systems.
Pneumocystis jiroveci, responsible for pneumonia, has become an increasingly common infection, especially in individuals with weakened immune systems, such as cancer patients undergoing immunosuppressive treatments like chemotherapy. Additionally, respiratory infections caused by the inhalation of spores from molds, particularly Aspergillus fumigatus and Aspergillus flavus, are prevalent among immunocompromised individuals.
C. neoformans stands out as the second most frequent opportunistic central nervous system infection in cancer patients, often leading to meningitis, with lymphoma patients being particularly at risk.
Candida spp., typically part of the microbiota in healthy individuals, can lead to opportunistic infections under suitable conditions. In addition to patient-related risk factors, the virulence characteristics of the fungus play a crucial role in the development of opportunistic infections. Factors such as broad-spectrum antimicrobial use, underlying diseases, patient age, the presence of medical devices in the body, adhesins, hydrolytic enzymes, and the ability to form biofilms contribute to the risk of fungal infections. The ability to form biofilms is especially significant in infections related to biomaterials. Urinary catheters, by providing a conducive environment for microbial biofilm development in terms of structural and surface conditions, are associated with various infections during prolonged use. While the removal of the biomaterial is recommended as the initial step in treating these infections, it may not be feasible for every patient, particularly in cases of hospitalized individuals.
Risk Factors Associated with Opportunistic Infections
Opportunistic infections are influenced by a myriad of risk factors categorized into three groups: biological factors, social and environmental factors. Biological factors are primarily associated with factors directly related to the host. Underlying diseases, genetic predisposition or defects, the presence of foreign material in the body, and antimicrobial usage are among the most significant contributors.
When discussing underlying diseases, diabetes emerges as a prominent example. Diabetes disrupts glucose balance in the body, with glucose being a crucial energy source for the development of fungi, especially Candida species. The presence of foreign materials, such as catheters, paves the way for Candida biofilm formation. The formation of biofilms diminishes the chances of antimicrobial success.
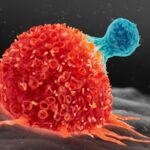
For cancer patients undergoing chemotherapy, the situation is challenging. Chemotherapy not only kills cancer cells but also leads to a 20% loss of healthy cells. This results in weakened immunity, rendering the patient vulnerable to infections. Moreover, chemotherapy can lead to sepsis, a condition known for abdominal infections caused by the loss of macrophages around the intestines. Sepsis is frequently observed as a side effect of chemotherapy in cancer patients, as the densest microbial flora is found in the colon, and macrophages in this region are particularly affected by chemotherapy.
Biological material extends beyond catheters, including pacemakers, catheters, dental and joint prosthetics, and intrauterine devices. These medical devices, like catheters, provide suitable surfaces for microbial adhesion and biofilm formation, leading to infections and reducing the success of antimicrobial treatments.
In addition to biological factors, it is well-established that environmental and sociocultural factors are linked to immune suppression and opportunistic infection development. Factors such as water and food contamination, inadequate hygiene among food and health workers, enclosed spaces (classrooms, offices), respiratory diseases, construction in the vicinity, animal bites, and the mixing of animal waste with water contribute to opportunistic infections within environmental factors. Poor nutrition, sleep deprivation, stress, smoking, alcohol use, and occupational factors also impact the immune system, falling under sociocultural factors.
Furthermore, certain occupations have been reported to increase the risk of specific diseases. Kim et al. (2017) conducted a study on wheat-related asthma risk in bakery workers, emphasizing that asthma in bakery workers is a wheat-related occupational disease. The study revealed a 3-17% incidence of upper respiratory infections and an 11-30% incidence of lower respiratory infections among bakery workers. Sensitivity to wheat flour ranged from 2-15%, influenced by exposure duration, work intensity, and genetic factors.
Wiggans et al. (2016) investigated occupational asthma in woodworkers. Coughing was the most frequently reported discomfort, affecting 6-80% of workers. Chest tightness, breathlessness, sputum production, and bronchitis were observed in varying percentages (9-40%, 10-39%, and 20-51%, respectively) among workers.
In summary, the development of opportunistic infections is a complex interplay of biological, social, and environmental factors, emphasizing the need for a holistic approach to managing and preventing these infections.