Respiratory Syncytial Virus (RSV) is one of the most common viruses worldwide that infects children and is increasingly recognized as a significant pathogen in adults, especially the elderly. The most common clinical scenario encountered in RSV infection is an upper respiratory tract infection; however, RSV typically manifests as bronchiolitis, a lower respiratory tract disease, in young children and can rarely progress to pneumonia, respiratory failure, apnea, and death.
Treatment for RSV is categorized into three main categories: supportive care, immunoprophylaxis, and antiviral drugs. The majority of RSV and bronchiolitis cases do not require specific medical intervention, and many treatments attempted thus far have been ineffective.
RSV is a common pathogen in humans due in part to the lack of long-lasting immunity after infection, leading to frequent reinfections. It infects approximately 90% of children within the first two years of life and often reinfects older children and adults.
Pathophysiology
RSV infection is limited to the respiratory tract. In infants or young children, the initial infection often affects the lower respiratory tract and typically presents as bronchiolitis, the clinical antithesis of upper respiratory symptoms. Viral transmission occurs in the respiratory epithelial cells of the upper respiratory tract. The spread of the virus down the respiratory tract occurs through intracytoplasmic bridges (syncytia) from cell to cell, originating from the upper respiratory tract to the lower respiratory tract (hence the name of the disease).
The disease may begin with upper respiratory symptoms and rapidly progress within 1-2 days to cough, nasal congestion, wheezing, and crackles, progressing to the development of diffuse small airway disease characterized by low-grade fever (<38.3C) and taken by mouth. There is often a family history of asthma or atopy. In more advanced disease, retractions and cyanosis may be observed, and up to 20% of patients may develop higher fever.
Apart from otitis media, which can occur in up to 40% of cases, the incidence of concurrent or secondary serious bacterial infections associated with RSV infection appears to be quite low. In very young infants, disproportionate apnea may be present with respiratory signs and symptoms, and a relatively nonspecific sepsis-like picture has been described in infants younger than 6 weeks old.
Reinfection with RSV can occur at any age; however, with recurrent infections and increasing age, the likelihood of RSV infections being limited to the upper respiratory tract is higher. RSV upper respiratory tract infection is proven to be more severe than the common cold, with a duration of illness lasting 7 to 10 days and evidence, such as findings from a study on RSV-infected adults, showing an average absenteeism from work of 6 days. Studies have also demonstrated severe RSV disease in elderly individuals.
Signs and Symptoms
Individuals infected with RSV typically exhibit symptoms within 4 to 6 days after infection. Symptoms of RSV infection commonly include:
Fever (often low-grade), Runny nose, Sneezing, Decreased appetite, Cough, Tachypnea (faster than normal breathing rate), Cyanosis (bluish discoloration), Sense of retractions or tightness in the chest, Wheezing, Sepsis-like presentation or episodes of apnea (in very young infants). These symptoms typically manifest in stages and may not all occur at once. In very young infants with RSV, the sole symptom may be irritability, decreased activity, and difficulty breathing.
Disease-Associated Genes, Causal Factors, and Risk Factors
Children with underlying conditions affecting cardiopulmonary function or immunity are likely to have an increased risk of developing severe RSV infection across all age groups. Among small children, those most frequently requiring hospitalization are premature infants and those with underlying chronic respiratory conditions such as bronchiolitis, cyanotic or complex congenital heart disease, immunosuppressive conditions, or other chronic illnesses affecting the processing of respiratory secretions.
Approximately one-third of children hospitalized for RSV infection in the first 5 years of life have one or more of these underlying conditions, a proportion that is higher in children older than 2 years. About one-quarter of children evaluated for RSV infection in pediatric clinics and emergency departments have a pre-existing chronic condition.
Early gestational age, with or without associated chronic lung disease, is a clearly significant risk factor for more severe RSV illness. Hospitalization rates for infants born before 36 weeks of gestation are three times or more higher than those born at term. As gestational age decreases below 32 weeks, the likelihood of admission with RSV infection increases, along with a substantial increase in the need for intensive care.
Recently, it has been recognized that late preterm infants (those with gestational ages between 33 and 35 weeks) with RSV infection disproportionately contribute to economic and clinical burdens, representing about three-quarters of all preterm infants. Compared to term-born infants, these late preterm infants not only significantly increase hospitalization costs and risks but also require substantially more medical resources for at least the following year.
Congenital heart diseases, particularly those accompanied by cyanotic heart diseases and conditions with pulmonary hypertension, rank among the top three conditions in infants hospitalized with RSV infection, requiring intensive care and mechanical ventilation in about one-quarter to one-third of cases. Infants hospitalized with unrepaired cyanotic congenital heart disease in the first few months of life are particularly vulnerable.
However, the increased rates of hospitalization for RSV due to congenital heart disease extend beyond infancy and are highest in the second year of life. Early surgical correction of cardiac defects has significantly reduced the mortality rate attributable to RSV infection from over 30% in the 1970s to below 2% today among infants with congenital heart disease.
Multiple demographic and environmental factors have also been evaluated for their role in increasing the risk of more severe RSV infection. Factors most commonly associated with RSV disease requiring hospitalization in young children include male gender, crowded living conditions, low socioeconomic status, exposure to other young children at home or in daycare, exposure to tobacco smoke, and lack of breastfeeding.
However, measuring the degree to which these factors play a role in the expression of RSV disease in children is challenging, and reported data are inconsistent and contradictory. The two most significant independent risk factors for hospitalization with RSV infection, particularly in the first 3 months of life, appear to be prematurity and young age.
An individual’s genetic background has significant but mostly unidentified effects on susceptibility to RSV infection and more severe disease. Certain racial and ethnic groups, notably Indigenous Native American and Alaska Native infants, including those living in the Yukon-Kuskokwim Delta region, have significantly increased rates of hospitalization and severe RSV infection, three to four times higher than observed in other U.S. infants. Severe disease from primary RSV infection has been linked to specific polymorphisms at specific genetic loci, affecting the expression of cytokines and inflammatory chemokines, impacting the immune response.
Virology
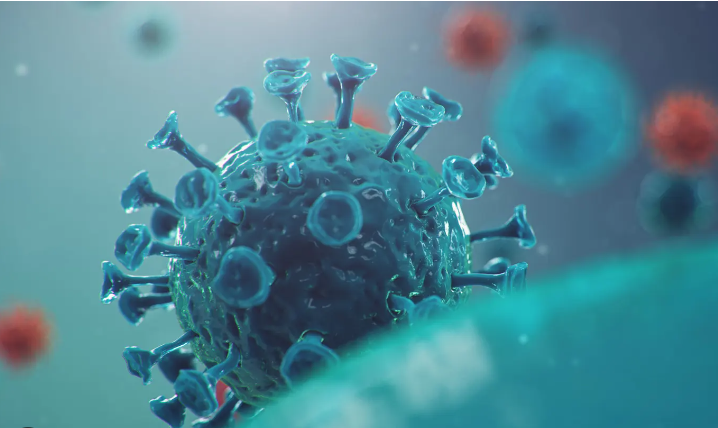
RSV was reclassified in 2016 into the Orthopneumoviridae genus within the Pneumoviridae family. Prior to this reclassification, the Pneumoviridae taxon was a subfamily within the Paramyxoviridae. RSV is a medium-sized (120-300 nm in diameter), pleomorphic enveloped virus with an unsegmented, negative-sense, single-stranded RNA genome (~15-16 kb) encoding 11 proteins, comprising two nonstructural and nine structural proteins. Among these proteins, G (attachment), F (fusion), and SH (putative viroporin) are hydrophobic transmembrane surface glycoproteins crucial for infectivity, as maximum efficient fusion requires the involvement of all three surface glycoproteins. These surface glycoproteins can also serve as targets for protective antibodies, making them potential therapeutic targets. G primarily mediates viral attachment to ciliated cells of the respiratory tract.

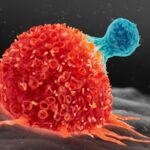
Source
Following attachment, F undergoes triggered structural changes into an activated form, facilitating viral penetration by fusing viral and host cell membranes and also promoting micropinocytosis. This also leads to the characteristic RSV syncytia, where infected cells fuse with neighboring uninfected cells, from which the virus derives its name. Both F and G proteins are antigens that elicit protective immunity and are crucial early targets for antibody-mediated neutralization of infection.
G exhibits moderate to high sequence diversity, defining antigenic groups A and B, whereas F is highly conserved among strains and widely recognized by cross-neutralizing antibodies, thus making it an attractive candidate as an RSV vaccine antigen. The pre-fusion form of the F protein is more effective at eliciting higher titers of neutralizing antibodies than the post-fusion form.
The M (matrix) protein accumulates on the inner surface of the envelope and is crucial for viral morphogenesis. Four nucleocapsid-associated proteins function as viral transcription factors: N (nucleoprotein), phosphoprotein (P), large (L), and M1-M2 proteins. Two nonstructural proteins, NS1 and NS2, can inhibit cellular type I interferon activity.
RSV isolates are further classified into two main antigenic groups, A and B, with A subdivided into 13 genotypes and B into 20 genotypes. The major genetic diversity between A and B, comprising approximately 50% genetic difference, is found in the G protein, followed by the M2 and SH proteins. Strains from both groups can circulate simultaneously during outbreaks, but the ratios and subtypes of A and B vary annually.
Pathogenesis
RSV infection is primarily acquired through close contact with an infected individual or direct inoculation of infectious secretions into the eyes and nose. Large particle aerosols generated by coughing and sneezing of an infected person can transmit RSV to others within approximately a one-meter radius. The spread of small particle (droplet nuclei) aerosols over longer distances appears to be much less likely. However, infection via touching objects contaminated with infectious secretions and then self-inoculation into the eyes or nose is a significant mode of transmission.
Experimental infection manifests in adult volunteers after an average incubation period of 3 to 5 days. Similarly, the average incubation period for naturally acquired infection appears to range between 2 to 8 days. The nasal and ocular mucosa seem to be equally sensitive entry portals, unlike the mouth. In hospitalized infants with primary RSV infection, peak viral titers range from 101 to 107 plaque-forming units (pfu)/mL of nasal secretion (averaging 105), gradually declining thereafter. The shedding period typically lasts 7 to 10 days, but the virus can sometimes be detected up to 30 days later. Increased viral load has variably been associated with greater disease severity.
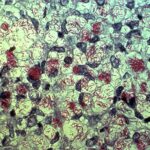
RSV replicates in the respiratory epithelium, primarily targeting ciliated columnar cells but may also involve additional cells such as type I and II pneumocytes. During primary infection, lower respiratory tract involvement typically presents as bronchiolitis, with initial pathological findings characterized predominantly by peribronchiolar infiltration of CD69+ monocytes with edema in the walls and surrounding tissue. Subsequently, characteristic proliferation and necrosis of the bronchiolar epithelium develop. The lumens of these small airways become obstructed due to shed epithelium and increased mucus secretion.
The airway of the small infant is particularly vulnerable to any degree of inflammation and obstruction because airway resistance is inversely proportional to the radius cubed. Airflow impedance occurs during both inspiration and expiration, but it is more pronounced during the latter as the lumen further narrows with positive expiratory pressure. Hence, hyperinflation arises from trapped air at the periphery of partially occluded areas. With complete occlusion, trapped air eventually gets absorbed, forming characteristic multiple areas of atelectasis.
The risk of developing such areas of atelectasis is high in small infants because collateral channels that preserve alveolar expansion in the presence of airway obstruction are not yet well-developed. These changes lead to an increase in lung volume and expiratory resistance. Infants with RSV-induced lower respiratory tract disease often exhibit pathological evidence for both pneumonia and bronchiolitis. Patients with pneumonia show interstitial infiltration of mononuclear cells, which can be accompanied by edema and areas of necrosis filling the alveoli. Most children with bronchiolitis show some histological signs of early healing within the first week of illness, characterized by the onset of regeneration of bronchiolar epithelium. However, ciliated cells may not be present for up to a week.
Immunity and Disease Pathogenesis
Various theories and supporting data have been presented to explain how RSV leads to these pathogenic manifestations. Most of our current understanding of the immunological responses to RSV stems from studies conducted in vitro and animal models. In humans, immune response cannot be dissociated from the perplexing and not fully understood effects of environment, age, antigenic experience, and genetics.
There is consensus that both viral and immunological mechanisms mediate the disease during primary infection. RSV produces its most devastating disease when specific antibodies derived from the mother are variably present. The severity of RSV infection in young infants with high levels of specific antibodies and the increased disease caused by the inactivated RSV vaccine developed in the 1960s initially suggested the singular role of the immune response in the pathogenesis of RSV in infants.
The potential importance of the host’s immune response to the development of the disease and subsequent long-term complications has further been supported by the observation that RSV is not highly invasive or cytopathogenic. While viral loads correlate with disease severity in humans, reducing viral replication through neutralizing antibody application targeting the F protein has not improved clinical illness in infants. However, recent data from murine models of RSV indicate that administration of non-neutralizing antibodies against the centrally conserved CX3C chemokine motif of the G protein can reduce inflammatory responses and disease even after infection has occurred.
Nevertheless, the relative contribution of immune response to the disease in infants has been questioned, particularly among children with bronchiolitis. It has been observed that RSV bronchiolitis children produce a stronger pro-inflammatory cytokine response compared to RSV-negative bronchiolitis children, but this has not been associated with more severe illness and has indeed been found to be protective against hypoxia.
Innate Immunity
The first line of defense against RSV infection in infants is the innate immune response initiated by the infection of the respiratory epithelium. RSV is a potent inhibitor of cellular antiviral type I interferons through the production of NS1 and NS2 proteins. Additionally, RSV interacts with Toll-like receptors (TLR) 2, 3, 4, and 7, triggering the release of inflammatory cytokines. Infection of the respiratory epithelium, antigen-presenting cells (dendritic cells), and macrophages results in numerous changes in gene expression, leading to the production of cell surface markers and the release of cytokines and chemokines. Inflammatory cells are recruited to the respiratory tract, including neutrophils, macrophages, mononuclear cells, T cells, natural killer (NK) cells, and eosinophils.
In infants with severe primary RSV infection requiring intubation, there is an early and robust neutrophilic infiltration into the airway, as determined by bronchoalveolar lavage, which is associated with a decrease in viral load before the development of T-cell responses. The variability in innate immune defense and the host’s susceptibility are increasingly associated with polymorphisms in genes that are integral components of innate immunity.
Diagnostic Methods
The specific diagnosis of RSV infection relies on the detection of the virus or viral antigens in respiratory secretions or the identification of virus-specific nucleic acid sequences. The type and quality of the clinical specimen significantly impact the results of all viral detection assays currently in use. Antigen-based tests are commonly available, easy to administer, and yield results quickly, but their decreased sensitivity and specificity are notable drawbacks.
Among the available methods, isolation in cell culture has been considered the gold standard for the sensitive identification of RSV, but it is gradually being replaced by highly sensitive and specific nucleic acid amplification assays, which provide faster results. New methodologies such as real-time PCR methods allow for the quantification of viral nucleic acids in clinical specimens. The disadvantages of nucleic acid-based assays include their high cost and limited standardization.
Laboratory Diagnosis
The specific diagnosis of RSV infection is made by detecting the virus or viral antigens or virus-specific nucleic acid sequences in respiratory secretions. The type and quality of the clinical specimen significantly influence the sensitivity and specificity of all currently available viral detection assays.
It has been shown that nasal wash fluid or nasopharyngeal aspirate is more sensitive in detecting RSV than a nasopharyngeal swab sample. However, obtaining a nasopharyngeal swab is much less discomforting for the patient, requires no special equipment, and can be performed in an outpatient setting as well. The use of newly designed flocked nasopharyngeal swabs, which effectively dislodge and collect virus-infected cells covering the nasopharynx, significantly enhances the quality of swab samples and therefore improves the diagnostic yield of the clinical specimen.
Laboratory methods currently available for the detection of RSV include:
- Virus isolation in tissue culture,
- Direct or indirect immunofluorescent staining (DFA/IFA) or enzyme-linked immunosorbent assays (EIAs) for the detection of viral antigens,
- Detection through nucleic acid amplification assays,
- Predominantly reverse transcription polymerase chain reaction (RT-PCR).
Differential Diagnosis
The differential diagnosis of RSV infection includes:
- Asthma
- Bronchiolitis
- Influenza
- Croup
- Bronchitis
- Pneumonia
Treatments or Management Methods
RSV treatment is divided into three categories: supportive care, immune prophylaxis, and antiviral drugs. The majority of RSV and bronchiolitis cases do not require specific medical intervention, and many treatments that have been tried throughout history have proven ineffective. RSV vaccines and therapeutic interventions for RSV continue to be the focus of intense scientific interest.
Preventive Measures
RSV transmission appears to occur through contact with infected secretions via hand-to-hand spread or contact with fomites and respiratory droplets, with an incubation period of 3-5 days. Aerosolized secretions seem to be less significant in RSV transmission; therefore, it is important to emphasize handwashing and cleaning surfaces in the environment to prevent RSV transmission. Isolating infected patients with RSV in hospital settings and wearing masks and gowns in close contact with infected children are important in controlling nosocomial spread. Pediatric units have been shown to be a significant concern for RSV transmission. Despite good environmental hygiene, RSV infection is likely to occur at a significant frequency.
If you have contact with a premature baby, a child with chronic lung or heart disease, or a child with a weakened immune system, you should take extra care to keep the baby healthy by:
- Wash Your Hands Frequently: Wash your hands often with soap and water for at least 20 seconds, and help small children do the same. If soap and water are not available, use an alcohol-based hand sanitizer. Washing your hands will help protect you from germs.
- Keep Your Hands Away from Your Face: Avoid touching your eyes, nose, and mouth with unwashed hands. Germs spread this way.
- Avoid Close Contact with Sick People: Avoid close contact with people who have cold-like symptoms, such as kissing them, sharing eating utensils, or eating with them.
- Cover Your Mouth and Nose When You Cough or Sneeze: Cover your mouth and nose with a tissue or your upper sleeve when you cough or sneeze. Then throw the tissue in the trash.
- Clean and Disinfect Surfaces: Clean and disinfect surfaces and objects that people frequently touch, such as toys, doorknobs, and mobile devices. Infected individuals can leave germs on surfaces and objects when they touch them. Additionally, droplets containing germs can land on surfaces and objects when they cough or sneeze.
- Stay Home If You Are Sick: If possible, take time off from work or school and stay home when you are sick; do not go to public places. This will help prevent others from getting sick.